
- #UHC MEDICARE ADVANTAGE TIMELY FILING LIMIT 2022 HOW TO#
- #UHC MEDICARE ADVANTAGE TIMELY FILING LIMIT 2022 CODE#
- #UHC MEDICARE ADVANTAGE TIMELY FILING LIMIT 2022 PLUS#
- #UHC MEDICARE ADVANTAGE TIMELY FILING LIMIT 2022 FREE#
In case, you’re looking for some additional information, feel free to contact us or comment below. In this article, I have mentioned everything you need to know about timely filing limit along with the timely filing limit of all major insurances in United States. Also ask your accounts receivable team to follow up on claims within 15 days of claim submission. If insurance company allows electronic submission then submit claims electronically and keep an eye on rejections. To avoid timely filing limit denial, submit claims within the timely filing limit of insurance company.
#UHC MEDICARE ADVANTAGE TIMELY FILING LIMIT 2022 HOW TO#
How to avoid from claim timely filing limit exhausted?
#UHC MEDICARE ADVANTAGE TIMELY FILING LIMIT 2022 CODE#
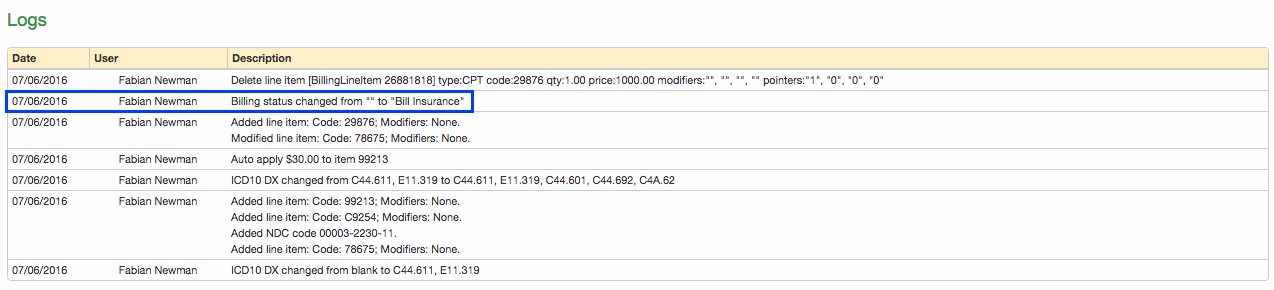
What if claim isn’t sent within the timely filing limit?įailing to submit a claim within the timely filing limit may result in the claim being denied with a denial code CO 29, so it is important to be aware of the deadline and submit the claim promptly. Unitedhealthcare Non Participating Providers Keystone First Resubmissions & Corrected Claimsġ80 Calender days from Primary EOB processing dateġ2 months from original claim determination
#UHC MEDICARE ADVANTAGE TIMELY FILING LIMIT 2022 PLUS#
If your Medicare Advantage health plan or your primary care provider decides, based on medical criteria that your situation is Time-Sensitive or if any physician calls or writes in support of your request for an expedited review, your Medicare Advantage health plan will issue a decision as fast as possible, but no later than seventy-two (72) hours - plus 14 calendar days, if an extension is taken - after receiving the request. your ability to regain maximum function.A Time-Sensitive situation is a situation where waiting for a decision to be made within the timeframe of the standard decision-making process could seriously jeopardize: You have the right to request and receive expedited decisions affecting your medical treatment in "Time-Sensitive" situations. Complaints and appeals may be filed over the phone or in writing. There is a lot of insurance that follows different time frames for claim submission. There is also a complaint process if you are not satisfied with the quality of services that you received from United Behavioral Health or your behavioral health practitioner. Timely Filing Limits for all Insurances updated (2023) Health (9 days ago) WebOne of the common and popular denials is passed the timely filing limit. United Behavioral Health offers an appeal process if you are not satisfied with a care advocacy or claims payment decision related to behavioral health services. You must include this signed statement with your appeal.Your representative must also sign and date this statement.Provide your Medicare Beneficiary Indentifier (MBI) from your member ID card.Provide your name, address and phone number and that of your representative, if applicable.(Note: You may appoint a physician or a Provider.) For example: “I appoint to act as my representative in requesting an appeal from your Medicare Advantage health plan regarding the denial or discontinuation of medical services.” Fill out the Appointment of Representative Form (PDF) and mail it to your Medicare Advantage plan or.Note: The sixty (60) day limit may be extended for good cause. You may appoint an individual to act as your representative to file the appeal for you by following the steps below: If you think that your Medicare Advantage health plan is stopping your coverage too soon.
Someone else may file the appeal for you on your behalf.An appeal may be filed by any of the following:


 0 kommentar(er)
0 kommentar(er)
